For those who menstruate, you know that your period is a monthly occurrence that lasts for 3-7 days. Your menstrual period occurs as a part of a longer female hormonal cycle called the menstrual cycle, which typically occurs over 28 days.
Your cycle is broken down into phases, and across these phases, your hormone levels change to prepare your body for the development and release of an egg, at which point you either become pregnant or if not, have your period.
At certain points throughout the cycle, these changes in hormones can make you more insulin resistant, and affect your glucose response. We’re going to walk you through the phases of your cycle, the hormonal changes that come with each phase, what impact you can effect these hormones to have on your insulin and glucose response, and what to do about it.
Phases of the menstrual cycle — and the hormones involved
There are four main hormones that drive your menstrual cycle: follicle-stimulating hormone (FSH), estrogen, luteinizing hormone, and progesterone [1].
These hormones ebb and flow throughout the phases of the menstrual cycle. Your cycle has four phases, some of which overlap.
- Menstruation phase: This is the first 5-7 days of your period. Estrogen, progesterone, FSH, and luteinizing hormone are low.
- Follicular phase: This phase starts on the first day of your period (overlapping with the menstruation phase) and goes until about midway through your cycle. During this time, estrogen levels rise as the body prepares eggs for release.
- Ovulation phase: This is when the egg is released from the ovary and moves through the fallopian tube to the uterus. This occurs around the 13-16th day of the cycle. Here, luteinizing and FSH are high, estrogen is low, and progesterone is rising [2]
- Luteal phase: This is the time right before your period when the uterine walls are thickening for the possibility of pregnancy if the egg is fertilized. In this phase, progesterone and estrogen are high, with progesterone at its peak. FSH and luteinizing hormones are low.
FSH, luteinizing hormone, estrogen, and progesterone are all essential to the phases of the cycle, but it is progesterone, estrogen, and the ratio of the two hormones that seem to have the most effect on glucose levels and insulin sensitivity.
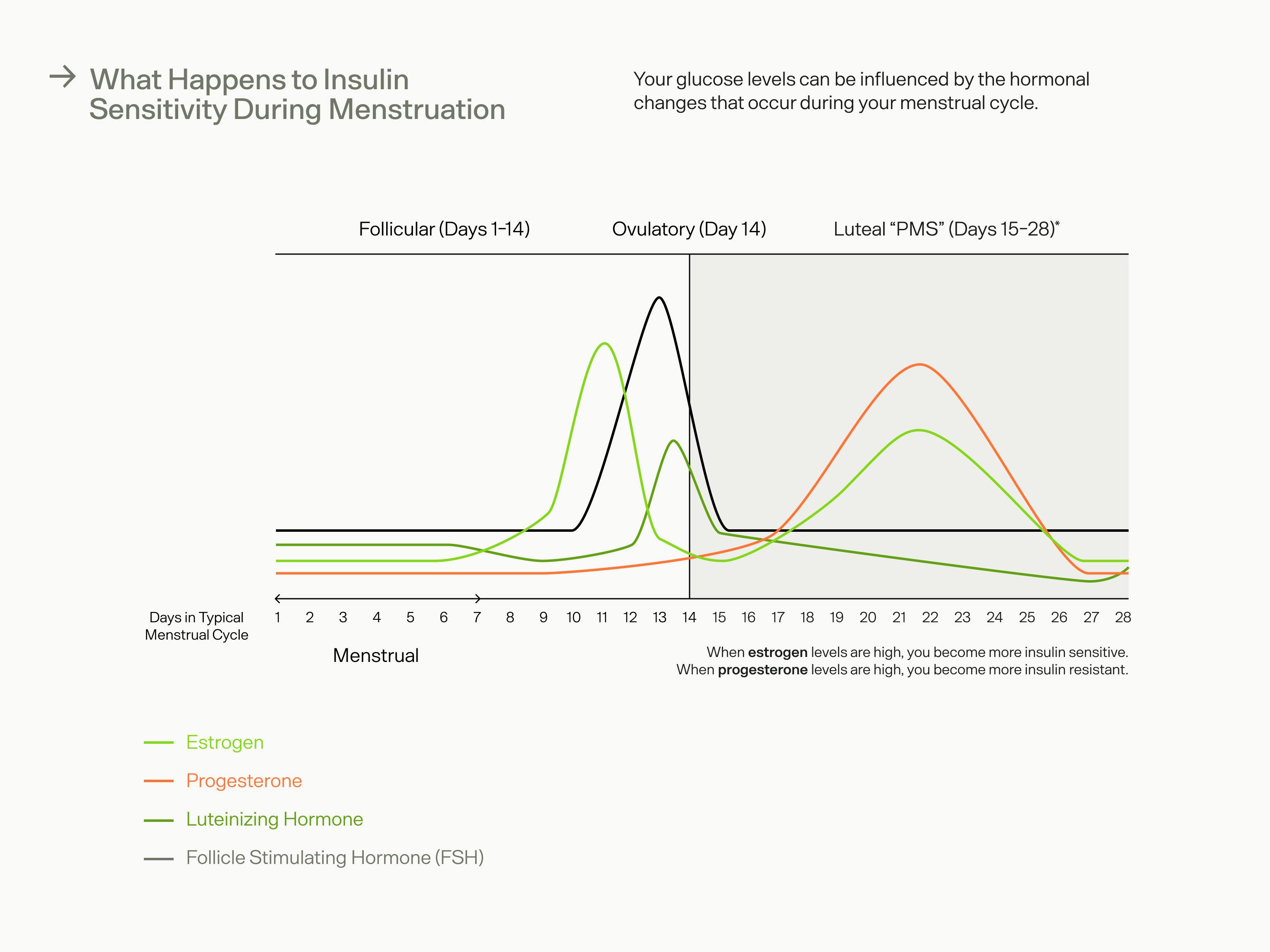
The hormones involved in your menstrual cycle — particularly estrogen and progesterone — can have an effect on your insulin sensitivity and glucose levels.
Can your period affect your blood sugar? Insulin sensitivity during menstruation
The luteal phase, or the “PMS” phase, is the phase where women may experience the most noticeable changes in blood sugar and insulin levels — especially women who experience strong PMS symptoms [3, 4].
During the luteal phase, when progesterone is at its highest and estrogen is high as well, research shows that women experience higher levels of circulating insulin, which is indicative of temporary insulin resistance during this phase [4].
Progesterone promotes the storage of glycogen in the liver, which is key for supporting pregnancy [5]. However, if you do not become pregnant during ovulation, this increase in progesterone will increase insulin resistance temporarily [6].
Estrogen, on the other hand, has been associated with improved insulin sensitivity and glucose in both animal and human studies [7, 8]. This suggests that the end of the follicular phase (second phase of the cycle) may be when you are most insulin sensitive, since estrogen levels are at their peak, and progesterone levels are low.
But what happens during the luteal phase, when both progesterone and estrogen are high? Scientists have found that higher levels of progesterone override the insulin-sensitizing effects of estrogen during this phase specifically.
What to do with this information
The luteal phase is when you may experience insulin resistance and elevated glucose. If you are concerned about blood glucose levels, try to avoid high-carb/high-sugar foods during this time, as they may have more of an impact on your blood sugar and insulin levels. You can also try some blood glucose hacks during this time for better glucose management.
That said, this phase is a normal part of your body’s physiology and the insulin resistance is temporary. It’s most important that you listen to your body and nourish yourself sufficiently with whole foods, adequate calories, and rest as needed.
Key Takeaways
Understanding the phases and hormonal fluctuations of your menstrual cycle can help you better understand blood glucose trends. Here are a few things to remember as you navigate your glucose management throughout your menstrual cycle:
- Your menstrual cycle goes through four phases: menstrual, follicular, ovulatory, and luteal.
- Progesterone and estrogen levels change throughout these phases and affect insulin sensitivity and blood glucose levels. The luteal phase when progesterone is highest is when you are most insulin resistant and may see higher glucose levels. The follicular phase, on the other hand, is when you are most insulin sensitive, due to high levels of estrogen and low levels of progesterone.
- During the luteal phase, focus on getting enough sleep, doing low-intensity exercise, and eating whole, colorful foods for better glucose management. Listening to your body is important during this phase, so take that extra rest if you need it — your body uses a lot of energy to prepare for menstruation.
- Monitor your blood glucose with a CGM to better understand your glucose trends throughout your cycle and better manage your health and self-care throughout.
References
- https://www.ncbi.nlm.nih.gov/books/NBK279054/
- https://www.merckmanuals.com/home/women-s-health-issues/biology-of-the-female-reproductive-system/menstrual-cycle
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3714432/
- https://academic.oup.com/jcem/article/95/12/5435/2835335
- https://pubmed.ncbi.nlm.nih.gov/7039319
- https://joe.bioscientifica.com/view/journals/joe/221/2/273.xml
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6341301
- https://ajp.amjpathol.org/article/S0002-9440(21)00245-5/fulltext


